In the last decade, there has been growing recognition of the importance of mental health economics, or the study of the economic impact of mental illness on individuals, families, communities, and society as a whole. After looking at the limitations of these economic evaluations in our previous issue of Invested, we are now delving into how far they have come in recent years.
To start, this quote from Knapp and Wong (2020) provides quite a succinct overview:
Mental health economics has developed rapidly over recent decades. From an earlier “age of innocence,” with apparently little recognition of resource scarcity by the research community, to a phase of “unbridled criticism,” which rejected economics as having any legitimate role to play in evaluating treatment and care…in terms of numbers, the cumulative total, or reports on economic evaluation of mental health care and treatment has grown from approximately 100 in 1999 to over 4,000 in 2019.
With institutions like the World Health Organization urging that economic evidence be a standard part of studies and proposals regarding mental health care and initiatives, as well as the impressive increase in number of economic studies, it seems safe to say that we have left the 'unbridled criticism' phase and are now perhaps in a phase of 'restrained praise.' Given the relatively small cost of adding an economic element and the relatively large impact it can have on the effectiveness of the outcome of decisions made, it makes sense for these evaluations to be the default option and not the exception.
Economic Impact Review
When we looked at the economic impact of mental illnesses and mental health care in a previous issue of Invested, we saw that it is by no means limited to a small group of predisposed individuals but is actually a major public health concern that affects all areas of the fabric of society. Medication, clinic visits, and hospitalizations are examples of direct economic costs, while loss of labour and income, strain on the education and judicial systems, and the financial, emotional, and time burden of caregivers are all examples of indirect costs.
Based on data from 2010, the global direct and indirect economic costs of the mental health disease group were estimated at US$2.5 trillion. Importantly, the indirect costs (US$1.7 trillion) are much higher than the direct costs (US$0.8 trillion) (Figure 1), which contrasts with other key disease groups, such as cardiovascular diseases and cancer. (Trauntmann, 2016)
Figure 1
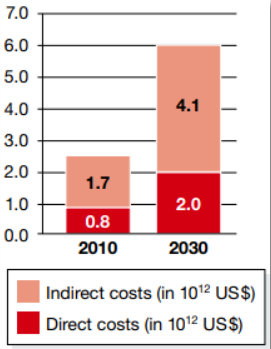
Source: Trauntmann 2016
Developments in Mental Health Economics
One of the most significant developments in this field has been bringing the focus of the economic burden of mental illness to the forefront of policy and decision-makers minds. Mental illness is a significant contributor to the global burden of disease and has a substantial economic impact in terms of health care costs, lost productivity, and decreased quality of life. As a result, policymakers and health care providers are increasingly recognizing the need to invest in mental health services and support. (Taylor, 2018)
Another important change is that there has been a shift away from a strict research focus of cost-of-illness numbers towards more cost-effectiveness analyses. There is now further movement towards the use of more patient-centered and holistic measures such as quality of life and functional outcomes, rather than just focusing on clinical measures. Along with this is the move to evaluate mental health interventions in the context of real-world settings, rather than just in controlled clinical trials. These measures all provide more meaningful, transferable, and relevant data. Demand for economic data has also moved away from being purely the domain of interest for commercial (i.e., pharmaceutical companies) and governments, to being utilized by hospitals and community outreach organizations, philanthropic foundations, and other social sectors like the judicial and education sectors. (Knapp & Wong, 2020)
Finally, that while in the previous issue of Invested, it was noted that many decision- and policy-makers work within shorter timelines, we must include here that there is a growing recognition of the importance of considering the long-term impacts of mental health interventions. There is no escaping the fact that mental health issues can have long-term effects on individuals and society. Economic evaluations that take a longer-term perspective can provide a more accurate picture of the costs and benefits of mental health care and treatment.
How Economic Impact is Measured
Along with classic economic analyses such as the cost-benefit and cost-effective analyses, Trauntmann at al (2016) describes a report from 2011 from the World Economic Forum that outlines three different approaches that can be used to quantify economic disease burden. When used together, these methods not only acknowledge hidden indirect costs, but also how a country's macroeconomic growth is impacted.
- The Human Capital Approach needs two kinds of data: (1) epidemiological which captures the prevalence of the disorder, number of people seeking treatment, associated mortality, disability, and imprisonment cases; and, (2) the economic data of per patient costs of the disorder. Epidemiological data is usually based on representative samples from a defined population, as well as cohort studies. The economic data is typically derived from statistics such as the average cost of a hospital bed per night. This is then multiplied with the corresponding epidemiological data.
- The Lost Economic Growth Approach is from a macroeconomic perspective and bases its findings on the fact that economic growth depends on labour and capital, which can both be negatively impacted by disease through disability and mortality and healthcare expenditures respectively. This is quantified by estimating the projected impact of mental disorders on a country's gross domestic product (GDP). The impact on labour is estimated by “comparing the GDP to a counterfactual scenario that assumes no deaths from a disease against the projected deaths caused by the respective disease.” (Trauntmann at al, 2016)
- The Value of Statistical Life Approach is the broadest and uses risk-value ratios. This method makes the assumption that trade-offs between risks and money can be used to quantify the risk of disability or death associated with mental disorders. Observed real-world, or hypothetical preferences gathered from surveys asking how much you would be willing to pay to avoid a particular risk, or conversely, how much money you would need to take on that risk, are used to calculate the risk-value ratios. For example:
Suppose that the average lifetime risk of dying from a depressive disorder is 15 in 1,000. Suppose further that there are measure that could reduce that risk to 5 in 1,000. If people of a certain population are willing to spend on average US$50,000 for these measures, VLS in that population would be US$5 million ($50,000/[(15-5)/1000]). The same logic can also be applied when evaluating the willingness to monetarily pay in order to avoid living with a certain disease. As a result, the VSL approach not only accounts for lost income and out-of-pocket spending on information, medications, and care, but also for costs that people associate with disability and suffering.(Trauntmann at al, 2016)
Overall, economic evaluations can provide valuable information to support decision-making across a range of areas, helping to ensure that mental health resources are allocated in the most effective and efficient way possible. If we continue to take these actions, society will hopefully be more willing to accept that spending money for preventing and treating mental disorders is a sustainable investment.
In the next issue of Invested, we will be concluding our series on mental health economics with a closer look at the ROI of some of Canada’s mental health initiatives.
Bibliography
[1] Knapp, M., & Wong, G. (2020). Economics and mental health: the current scenario. World Psychiatry, 19(1), 3-14.
[2] Taylor, H. G. P. (2018). Helping to Improve the Mental Health of Canadians. Canadian Journal of Community Mental Health, 36(Special Issue), i-iv.
[3] Trautmann, S., Rehm, J., & Wittchen, H. U. (2016). The economic costs of mental disorders: Do our societies react appropriately to the burden of mental disorders?. EMBO reports, 17(9), 1245-1249.